What’s the diagnosis?
Pustules with scarring alopecia

Figure 1. Multiple small follicular cysts, papules, pustules and patchy scarring on the occipital area.
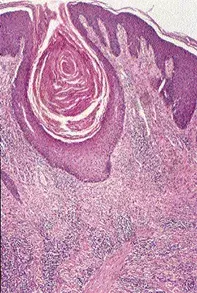
Figure 2. Scalp biopsy demonstrating a dilated follicular canal filled with keratin, and surrounding fibrosis, plasma cells and hair granulomas.
Differential Diagnosis
Tinea may present with follicular pustules and broken hairs as well as large exudative nodules (kerion). Examination of the hair shafts and fungal cultures may confirm the diagnosis.
Tufted hair folliculitis is associated with scarring alopecia and grouped hairs which emerge as distinct tufts. In some individuals tufted hair folliculitis is a primary disorder, but it may also be seen as a secondary event in scarring alopecias associated with a wide range of pustular conditions.
Folliculitis decalvans is a progressive scarring alopecia which is associated with follicular pustules at the active enlarging edge. The same process may involve the beard. It is thought to be due to Staphylococcus aureus folliculitis complicated by a marked immunological reaction to this organism.
Dissecting cellulitis of the scalp is a disorder seen particularly in black men. It is associated with multiple deep abscesses which are fluctuant and associated with draining sinuses as well as ulceration.
Folliculitis keloidalis (acne keloidalis nuchae) is the correct diagnosis in this case. It is characterised by multiple follicular papulopustules which progress to gross scarring, and is particularly located on the occipital area and nape of the neck. On scalp biopsy, the presence of dilated follicular canals filled with keratin, as well as the follicular perforation by hair, may be clues to the diagnosis. Acute and chronic folliculitis with abscesses and granulomas are often evident. Cultures often grow Staphylococcus aureus. In black men, close shaving of the occipital hair may result in follicular perforation by curled hairs and thus may contribute to this condition.
Treatments include tetracycline, doxycycline or cephalexin and intralesional corticosteroids. In some patients surgical removal of the involved skin may be the treatment of choice, particularly when the process is very active and destructive and not responding to treatment or to remove hypertrophic scar tissue.
A 35-year-old black man presented with multiple papulopustules located predominantly on the occipital area of his scalp (Figure 1). The pustules had been present for about two years and had resulted in a patchy scarring alopecia. Skin biopsy showed extensive dermal fibrosis as well as a dilated follicular canal filled with keratin (Figure 2). The scar tissue showed prominent plasma cells and there were loose hair shafts in the dermis associated with a granulomatous reaction. Stains for fungi were negative.