What’s the diagnosis?
Acral blisters with arthritis

Epidermolysis bullosa is a heterogeneous group of inherited disorders that are characterised by mutations in adhesion molecules or anchoring fibrils that bind the skin. These disorders usually appear in early life. Mild forms may present as fragile skin with superficial blisters of the feet and hands, particularly the soles and palms. Skin biopsy may show dissolution of basal keratinocytes due to abnormalities in keratin tonofilaments, important in keratinocyte adhesion structures in the basal layer.
Bullous pemphigoid may present with acral blisters but is usually more generalised. The individual lesions arise on an urticarial base. Skin biopsy shows a subepidermal blister with eosinophils and is rarely cell-poor. Skin immunofluorescence reveals linear deposits of immunoglobulins along the basement membrane zone.
Porphyria cutanea tarda presents in an identical clinical and histological pattern to that seen in this case. It is associated with elevated porphyrins produced by the liver, which can be tested by quantitating urinary porphyrins. Porphyria cutanea tarda is aggravated by excess iron and oestrogens.
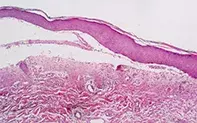
Pseudoporphyria is the correct diagnosis. A skin biopsy revealed a subepidermal blister with scant dermal inflammation (Figure 2). It may be induced by a variety of drugs, including naproxen, nalidixic acid, tetracyclines, frusemide and retinoids. Pseudoporphyria may also be seen in acral areas in individuals who have chronic renal failure, with or without dialysis, and in those with chronic sun damage or chronic UV exposure via tanning beds. A careful drug history and a history of exposure to sunlight or artificial light are important in reaching a diagnosis. Porphyrin studies are required to exclude porphyria cutanea tarda. Naproxen-induced blisters are seen particularly in children and may be associated with pitted angular or linear facial scarring. Treatment Removal of the offending agent usually results in slow resolution of the blisters over several months. Sun protection will be required. Other nonsteroidal anti-inflammatory drugs, such as diclofenac, indomethacin or COX-2 inhibitors, may be substituted for naproxen.
Over a two-month period, a 52-year-old woman developed bilateral nonpruritic blisters (Figure 1) and fragile skin, localised to the dorsal surfaces of her hands. The individual blisters healed with scars. Over the preceding six months, the patient had been taking naproxen for arthritis. She had a background of chronic solar damage.